|
Simulation Characteristics |


 |
The characteristics of the simulation under assessment must be
considered because they help make design choices - both the type of
evaluation conducted as well as the planning and execution of the
planning evaluation.
The
following simulation taxonomy leverages simulation categories defined by
Alinier (2007) to differentiate simulators along a variety of
significant dimensions.
| |
Low Fidelity |
Intermediate
Fidelity |
High
Fidelity |
| |
Level 0
Written
Simulations |
Level 1
Patient
models |
Level 2
Screen based
Simulators |
Level 3
Intermediate
fidelity patient simulators |
Level 4
Interactive
patient simulators |
Level 5
Immersive
Scenario Support
simulation |
|
Description |
Paper-based
simulations |
Basic
mannequin, low fidelity simulation models, part task
simulators that model specific procedures and body parts.
Provide a visual experience, augmented with haptic
capabilities. |
Computer/PDA in
networked or standalone mode with simulation software such
as games, videos, Virtual Reality and surgical simulators.
|
Computer
controlled programmable full body size patient simulators.
Not fully interactive. |
High fidelity,
computer controlled, model driven patient simulators with
accurate physiological models for different patients and
scenarios. Fully interactive. |
Patient
fidelity
Environmental
Fidelity |
|
Typical Uses
|
Instruction
–
Didactic
Learning
Demonstration
–different scenarios
|
Demonstration
Practice-
individual
skill acquisition |
Instruction
–
Didactic
Learning
Practice
– scenarios
involving multiple skills
Feedback-
during scenario or automated After Action Review
|
Demonstration
Practice
–
Lane training
Large scale
training exercises
Feedback
– patient response, instructor |
Demonstration
Practice
–
Lane training
Large scale
training exercises
Feedback
– patient response, instructor |
Practice -
Lane training
Large scale
training exercises |
|
RDECOM Product
Examples |
·
Combat Medic Card Game |
·
STAT trainer |
·
TC3 Simulation
·
Mobile Medic
·
Nexus |
·
Stand Alone Patient Simulator
|
|
Patient
fidelity:
·
Prosthetics
·
Olfactory
Cues
·
TraumaFX™
·
Simulated
Bilogical Tissue
Environmental:
fidelity:
·
Scent
·
STS mobile MSTC |
|
Skills
|
Cognitive |
cognitive,
psychomotor
|
cognitive
|
cognitive,
psychomotor, psychosocial, team |
cognitive,
psychomotor, psychosocial, team |
N/A…
Familiarization
/ habituation |
|
Assessment
|
Cognitive
test-declarative & procedural knowledge |
Cognitive test-declarative
& procedural knowledge;
Hands on
performance
Behavioral
observation;
Objective
performance \measurement (e.g., simulation log of time to
compress artery) |
Cognitive test
-declarative & procedural knowledge
Objective
performance measurement (e.g., time, procedural knowledge) |
Cognitive test-declarative
& procedural knowledge;
Hands on
performance-
Behavioral observation; Objective performance measurement
(e.g., time, proper location) |
Cognitive test-declarative
& procedural knowledge;
Hands on
performance-
Behavioral observation; Objective performance measurement
(e.g., time, proper location) |
|
|
Automated
Performance Measurement |
Low
(e.g., may
involve computer administered assessment) |
Low
(e.g., may
involve computer log) |
High
Computer log
(e.g., accuracy of procedures and triage decisions, Decision
making time, tests) |
Moderate to
High
Computer log
(e.g., patient outcomes, speed/time, accuracy of
interventions) |
High
Computer log
(e.g., patient outcomes, speed/time, accuracy of
interventions) |
|
|
Facility
|
Classroom |
Classroom,
Trauma lane |
Classroom,
Computer lab |
Classroom,
Trauma lane, Field |
Classroom,
Trauma lane, Field |
Specialized lab
(e.g., ventilated rooms), Trauma lane, Field |
|
Typical Delivery |
student led |
student or
trainer led |
student or
trainer led |
trainer led |
student led |
student led |
|
Mobile delivery |
Low
|
Moderate |
Low to moderate |
Moderate to
High
Tethered
|
High
Wireless |
High
|
The type of simulation impacts the
evaluation protocol used. For instance, while there are general
usability questions that always apply, what they translate to for a
manikin is not the same as a screen based simulation (e.g. computer or
video).
The type of skill being taught impacts what
type of training makes the most sense. For instance, complex psychomotor
skills are not best taught, or for that matter assessed, by simply
asking trainees to describe how they would conduct it.
Whether or not a system has automated
performance assessment also impacts the protocol, because it effects
what data is automatically collected and available for analysis.
The interactivity of a system impacts the
evaluation protocol, because it effects the type and variation of user
actions and system responses that need to be considered.
The mobility of the system is important
because it impacts the accessibility of the system and the number and
type of contexts that might be considered for evaluation. When the
simulation is not stationary during training there can be significant
technical/manpower challenges unless there is automated performance data
collection.
For instance, consider the basic
characteristics of the following RDECOM STTC sponsored projects and the
impact of differences between them:
|
RDECOM STTC Projects |
|
 |
Combat Medic Card Game
The Combat Medic Card Game provides a
portable and inexpensive avenue for Combat Lifesavers and
Combat Medics to continue to reinforce training skills for
medical emergencies without the presence of instructors. The
card game is easy to play and can be modified into many
different types of games to be played individually or in
teams.
The card game focuses the top three
battlefield injury conditions: hemorrhage control,
obstructed airway and tension pneumothorax due to chest
wounds. By providing an opportunity to continue training,
the card game helps increase the chances of survival for
those injured by keeping the most common battlefield
injuries highlighted for the Combat Lifesaver and Combat
Medic.
http://www.rdecom.army.mil/STTC/FactSheetCombatMedicCardGame.pdf
|
|
 |
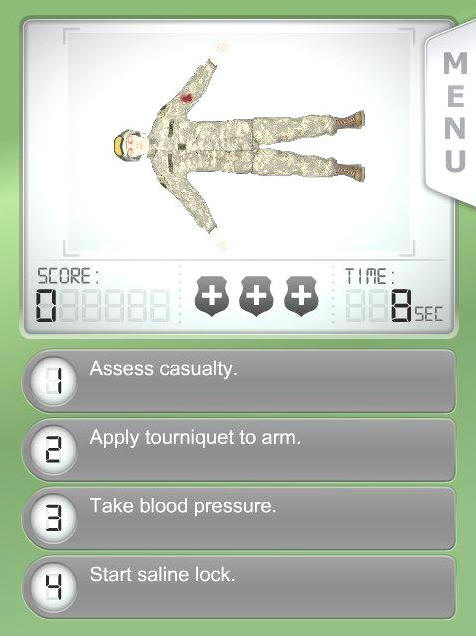
Tactical Combat Casualty Care (TC3)
Simulation
The Tactical Combat Casualty Care (TC3)
Simulation is a game engine-based technology to provide an
engaging, relevant, virtual training environment for
training Army Combat Medics. Trainees are immersed in a
realistic virtual scenario and must demonstrate both their
Soldier and technical medical skills to successfully
complete the training event.
http://www.rdecom.army.mil/STTC/FactSheetTC3.pdf |
|
 |
TraumaFX™
TraumaFX™ is an end-state high fidelity prototype of a lower
body injury using stateof-the-art special effects
technology. Hemorrhage control is the most important life
saving aspect in battlefield Medicine. A Soldier can go into
hypovolemic shock and bleed to death within minutes after
injuring a large blood vessel. Severe trauma caused to
extremities produce major challenges to our front line
Medics as they are not mentally, psychologically and
technically prepared to treat such disturbing wounds.
TraumaFX™ can be worn by human patient simulators or human
actors to support realistic hemorrhage control training. The
simulator includes an upper body with a penetrating wound on
the chest to prompt treatment with a chest seal.
http://www.rdecom.army.mil/STTC/FactSheetTraumaFX.pdf |
|
 |
Stand Alone Patient Simulator
Researched and developed under an Army
Technology Objective (ATO), the Stand Alone Patient
Simulator (SAPS) introduces the capability for medical care
providers to train as they fight. The provider must assess
and treat the patient in difficult terrain while extricating
and evacuating him to higher levels of care. Medics must now
master the skills required for care under fire and tactical
field care with patients that can die if not treated
correctly. The simulation provides medical educators and
instructors with the capability to objectively evaluate
student performance through the implementation of valid,
accurate and repeatable medical simulations that eliminate
subjective influences in simulation outcomes and in
assessment of student performance. This allows the SAPS to
be used both for proficiency and competency-based training.
http://www.rdecom.army.mil/STTC/FactSheetSAPS.pdf
|
|
 |
Olfactory Cues for Medical Training
Studies have shown the sense of smell
triggers emotional response usually as great as or greater
than that triggered by other senses. The incredible blend of
odors in the environment can overwhelm a Warfighter; add the
biological-based smells due to injuries and an inexperienced
Combat Medic, Combat Lifesaver or Corpsman can be rendered
ineffective.
By leveraging commercial off-the-shelf
technologies and custom-developed hardware and software,
Research, Development and Engineering Command, Simulation
and Training Technology Center (RDECOM STTC) hopes to show
that when students are exposed to malodors prior to
immersive training events, they will be more effective in
the actual event.
http://www.rdecom.army.mil/STTC/FactSheetOlfactoryCues.pdf
|
|
 |
Mobile Medic
The Combat Lifesaver (CLS) Classroom
Training Application or Mobile Medic is a mobile training
application for assisting student understanding of course
material during the CLS course. When used with existing
skill labs, it will allow students to become more familiar
with fundamental skills while allowing instructors to focus
on more advanced procedures during the skill lab. The
application is designed to be used in a 5-10 minute window
between the presentation of classroom material and a skill
lab for minimal impact to the overall length of the CLS
course.
http://www.rdecom.army.mil/STTC/FactSheetMobileMedic.pdf |
|
 |
Simulated
Biological Tissue
Requirements to increase
the trauma and surgical skills of military medical personnel
have resulted in significant increases in the use of live
tissue in training. Even though these training efforts have
improved the survival chances of wounded Soldiers in the
field they are unsustainable as long term solutions.
RDECOM STTC is leading
a multi-agency effort to develop simulation technologies
that will reduce the military’s reliance on live animals and
on cadavers to train surgical and trauma treatment skills.
http://www.rdecom.army.mil/STTC/FactSheetLiveTissueReplacement.pdf |
|